Black Maternal Mortality: A Public Health Crisis
- Feb 18, 2021
- 4 min read
What is Maternal Mortality?
Relevant definitions and information
The World Health Organization classifies maternal mortality as "the death of a woman while pregnant or within 42 days of termination of pregnancy, from any cause related to or aggravated by the pregnancy or its management but not from accidental or incidental causes." (Maternal mortality: Levels and trends, 2019) From this definition, maternal deaths can be recorded as either a direct or indirect maternal cause. Direct maternal death arises from obstetric complications in the pregnant state*, including hypertensive disorders, anesthetic complications, and difficult cesarean sections. Indirect maternal deaths are those resultant from diseases (pre-existing or otherwise) exacerbated by the physiologic effects of pregnancy. For example, many women with cardiovascular morbidity experience an increased risk of mortality due to maternal hemodynamic* changes.
The History of Black Maternal Mortality in the U.S.
Institutional racism and reproductive oppression
J. Marion Sims, the founding father of gynecology, created his legacy by surgically experimenting on non-consenting, enslaved Black women. Sims perpetuated the racist notion that Black people cannot feel pain like white people and refused anesthesia for the surgical procedures he performed. Certainly, then, we must acknowledge the role of slavery and the dehumanization of Black bodies in the field of obstetrics and gynecology.
Harriet Washington stated that “enslavement could not have existed and certainly could not have persisted without medical science. However, physicians were also dependent upon slavery, both for economic security and for the enslaved “clinical material” that fed the American medical research and medical training that bolstered physicians’ professional advancement.” (Washington, 2007)

J. Marion Sims; founding father of gynecology
New York Public Library
The fertility of enslaved Black women was used to build capital for slave-owners. Invasive gynecological experimentation allowed for the continued use of Black bodies as capital. Racism, past and present, is a stressor that reveals itself at physiological and genetic levels. Therefore, we see this history in our statistics today. Systemic racism can be seen in every facet of the U.S., institutionally embedded into our education. The legacy of racism and slavery, in medical experimentation, functions foundationally in every failure we make to close racial gaps in care and health outcome.
What Does Black Maternal Mortality Look Like in the U.S.?
Facts and statistics
Maternal Mortality Ratio (MMR) is defined by the number of maternal deaths per 100,000 live births during a given time interval. Maternal Mortality Rate (MMRT) is the average number of maternal deaths in a population divided by the average number of women at reproductive age during a specific observation period. Additionally, MMRT reflects both live births and stillbirths and can reveal maternal death risk per pregnancy or per birth as well as the population's fertility level.
From 2007 to 2016, the number of pregnancy-related deaths were measured by the Centers for Disease Control and Prevention to be:
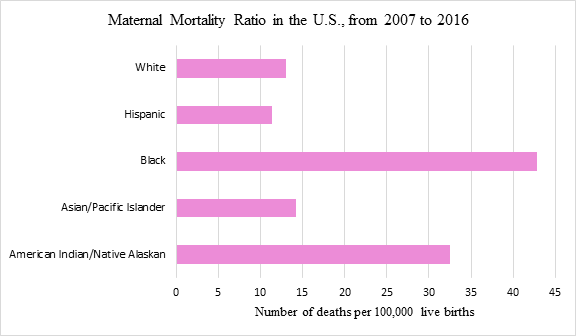
Center for Disease Control and Prevention
This means that Black women experienced an MMR of 42.8 (or 42.8 deaths per 100,000 live births) while white women had a calculated MMR of 13 (or 13 deaths per 100,000 live births). According to the CDC, postpartum hemorrhage, severe hypertension, and venous thromboembolism are the most common potentially preventable causes of maternal mortality. Venous thromboembolism causes as many as 180,000 deaths annually, many of which are preventable. Blacks have the highest rates of risk. Additionally, the Jackson Heart Study revealed a link between stress and the risk of developing hypertension. Black individuals are exposed to higher stress-levels than whites over the lifetime due to racism, thus increasing their risk of morbidity. Through the years, Black maternal mortality has presented at a steady rate of around 3 to 4 times higher than that of white maternal mortality. It must also be acknowledged that American Indian and Native Alaskan populations are not far behind, with an MMR of 32.5 from 2007 to 2016. This can be accounted for by ethnocentric* practices in the United States that seek to erase Native culture as well as the racism experienced since colonization.
Data collected in 2018 fares no better, with Black women still leading in the highest rate of pregnancy-related deaths in the United States. The MMR was determined to be 37.1 for Black women and 14.7 for white women. For further comparison, the CDC and NCHS reports that “the national maternal mortality rate in the U.S. for 2018 was 17.4 maternal deaths per 100,000 lives births.” (Center for Disease Control and Prevention, 2020) The numbers follow a historic trend and are not soon to change if Black women are not provided equitable access to resources such as quality prenatal care. Changes must be made at the institutional level in order to eradicate racial bias in medicine.
Maternal mortality trends in the United States, as well as in many other parts of the world, is a public health crisis. Needless, countless deaths occur as a result of continued failures to perform medicine with a deracialized view. To make a change, incoming medical professionals must learn from the mistakes of a racially biased establishment and do better to close the racial health gap. That is, the medical institution must be dismantled and reformed in textbooks and practice to focus on all patients equally; to acknowledge but not continue supporting a system so deeply rooted in racism.
What Can You Do?
1. Support Black youth as medical professionals
Follow: @thepediatricplayground on Instagram
Follow: @melanin.in.medicine on Instagram
2. Sign petitions to allow doulas support in hospitals during COVID-19
Doulas are essential to closing the racial maternal mortality gap
3. Spread the word! It’s important to increase awareness of maternal mortality as a public health crisis
*Vocabulary
Hemodynamic: relating to or functioning in the mechanics of blood circulation
Pregnant state: pregnancy, labor, and puerperium*
Puerperium: the period between childbirth and the return of the uterus to its normal size
Ethnocentric: characterized by or based on the attitude that one’s own group is superior
All definitions retrieved from https://www.merriam-webster.com/



Comments